WHAT IS A COLONOSCOPY?
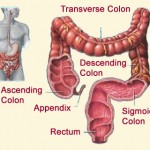
A colonoscopy is an outpatient procedure in which the inside of the large intestine (colon and rectum) is examined. A colonoscopy is commonly used to evaluate gastrointestinal symptoms, such as rectal and intestinal bleeding, abdominal pain, or changes in bowel habits. Colonoscopies are also performed in individuals without symptoms to check for colorectal polyps or cancer. A screening colonoscopy is recommended for anyone 50 years of age and older, and for anyone with parents, siblings or children with a history of colorectal cancer or polyps.
WHAT HAPPENS BEFORE A COLONOSCOPY?
To complete a successful colonoscopy, the bowel must be clean so that the physician can clearly view the colon. It is very important that you read and follow all of the instructions given to you for your bowel preparation well in advance of the procedure. Without proper preparation, the colonoscopy will not be successful and the test may have to be repeated.
If you feel nauseated or vomit while taking the bowel preparation, wait 30 minutes before drinking more fluid and start with small sips of solution. Some activity (such as walking) or a few soda crackers may help decrease the nausea you are feeling. If the nausea persists, please contact your health care provider.
You may experience skin irritation around the anus due to the passage of liquid stools. In order to prevent and treat skin irritation, you should:
- Apply Vaseline or Desitin® ointment to the skin around the anus before drinking the bowel preparation medications; these products can be purchased at any drug store.
- Wipe the skin after each bowel movement with disposable wet wipes instead of toilet paper. These are found in the toilet paper area of the store.
- Sit in a bathtub filled with warm water for 10 to 15 minutes after you finish passing a stool; after soaking, blot the skin dry with a soft cloth, apply Vaseline or Desitin ointment to the anal area, and place a cotton ball just outside your anus to absorb leaking fluid.
WHAT HAPPENS DURING A COLONOSCOPY?
During a colonoscopy, an experienced physician uses a colonoscope (a long, flexible instrument about 1/2 inch in diameter) to view the lining of the colon. The colonoscope is inserted into the rectum and advanced through the large intestine. If necessary during a colonoscopy, small amounts of tissue can be removed for analysis (a biopsy) and polyps can be identified and entirely removed. In many cases, a colonoscopy allows accurate diagnosis and treatment of colorectal problems without the need for a major operation.
- You are asked to wear a hospital gown and remove eyeglasses.
- You are given a pain reliever and a sedative intravenously (in your vein); you will feel relaxed and somewhat drowsy.
- You will lie on the left side, with your knees drawn up towards your chest.
- A small amount of air is used to expand the colon so the physician can see the colon walls.
- You may feel mild cramping during the procedure; cramping can be reduced by taking slow, deep breaths.
- The colonoscope is slowly withdrawn while the lining of your bowel is carefully examined.
- The procedure lasts from 30 minutes to one hour.
WHAT HAPPENS AFTER A COLONOSCOPY?
- You will stay in a recovery room for observation until you are ready for discharge.
- You may feel some cramping or a sensation of having gas, but this quickly passes.
- If medication has been given, a responsible adult must drive you home; avoid alcohol, driving, and operating machinery for 24 hours following the procedure.
- Unless otherwise instructed, you may immediately resume your normal diet, but we recommend you wait until the day after your procedure to resume normal activities.
- If polyps were removed or a biopsy was taken, avoid taking aspirin, products containing aspirin, or anti-inflammatory drugs (such as ibuprofen [Advil®, Motrin®], naproxen [Naprosyn®] or indomethacin [Indocin®]) for two (2) weeks after the procedure to help decrease the risk of bleeding; you may take acetaminophen (such as Tylenol®) if needed.
- If you are taking Coumadin®, Plavix®, Ticlid®, or Agrylin®, the physician performing your colonoscopy will advise you when it is safe to resume your blood thinners.
- If a biopsy was taken or a polyp was removed, you may notice light rectal bleeding for one to two days after the procedure; large amounts of bleeding, the passage of clots, or abdominal pain should be immediately reported.